ABSTRACT
Background
Little is known about the differences between physicians in training and post training in their willingness to comply with patient requests at the end of life.
Objective
To compare the attitudes of attendings and residents regarding a range of patient requests at the end of life
Design
Written, cross-sectional survey
Participants
The cohort included 191 attendings randomly selected across the state of Connecticut and 240 residents from 2 university-affiliated Internal Medicine programs.
Main Measures
We surveyed attendings and residents about their willingness to honor the requests of the same decisionally capable elderly patient in five scenarios involving different requests regarding end-of-life treatment.
Results
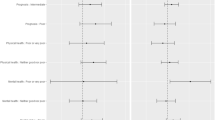
While a large majority of both attendings and residents were willing to comply with each of the requests to withhold intubation (100 % and 94 %, respectively), to extubate (92 % and 77 %), and to give increasingly higher doses of narcotics (94 % and 71 %), a significantly larger proportion of attendings versus residents was willing to comply with each of these requests. Small proportions of attendings and residents were willing to prescribe a lethal amount of sleeping pills (3 % and 5 %, respectively) and to give a lethal injection in its current illegal state (1 % and 4 %). A significantly larger proportion of residents (32 %) compared to attendings (19 %) was willing to give a lethal injection if legal. Adjusting for sociodemographic factors, attending status was independently associated with willingness to extubate [adjusted odds ratio (AOR) = 3.0, 95 % CI = 1.6-5.7] and to give a lethal injection if legal (AOR = 0.5, 95 % CI = 0.3-0.8). The proportion of physicians willing to extubate increased across years since graduation, with the greatest differences occurring across the residency years (69 % to 86 %).
Conclusions and Relevance
Clinical experience was an important determinant of physicians’ willingness to perform multiple patient requests at the end of life, with substantial changes in attitudes occurring during residency training. More research is needed to determine whether dedicated clinical exposure for physicians in training influences attitudes.
Similar content being viewed by others
References
Farber NJ, Simpson P, Salam T, Collier VU, Weiner J, Boyer EG. Physicians' decisions to withhold and withdraw life-sustaining treatment. Arch Intern Med. 2006;166(5):560–4.
Caralis PV, Hammond JS. Attitudes of medical students, housestaff, and faculty physicians toward euthanasia and termination of life-sustaining treatment. Crit Care Med. 1992;20(5):683–90.
Christakis NA, Asch DA. Biases in how physicians choose to withdraw life support. Lancet. 1993;342(8872):642–6.
Christakis NA, Asch DA. Physician characteristics associated with decisions to withdraw life support. Am J Public Health. 1995;85(3):367–72.
Hanson LC, Danis M, Garrett JM, Mutran E. Who decides? Physicians' willingness to use life-sustaining treatment. Arch Intern Med. 1996;156(7):785–9.
Fried TR, Stein MD, O'Sullivan PS, Brock DW, Novack DH. Limits of patient autonomy. Physician attitudes and practices regarding life-sustaining treatments and euthanasia. Arch Intern Med. 1993;153(6):722–8.
Emanuel EJ, Fairclough DL, Daniels ER, Clarridge BR. Euthanasia and physician-assisted suicide: attitudes and experiences of oncology patients, oncologists, and the public. Lancet. 1996;347(9018):1805–10.
Wolfe J, Fairclough DL, Clarridge BR, Daniels ER, Emanuel EJ. Stability of attitudes regarding physician-assisted suicide and euthanasia among oncology patients, physicians, and the general public. J Clin Oncol. 1999;17(4):1274.
Shapiro RS, Derse AR, Gottlieb M, Schiedermayer D, Olson M. Willingness to perform euthanasia. A survey of physician attitudes. Arch Intern Med. 1994;154(5):575–84.
Bachman JG, Alcser KH, Doukas DJ, Lichtenstein RL, Corning AD, Brody H. Attitudes of Michigan physicians and the public toward legalizing physician-assisted suicide and voluntary euthanasia. N Engl J Med. 1996;334(5):303–9.
Bushwick B, Emrhein D, Peters K. A comparison of resident and faculty attitudes toward physician-assisted suicide and active voluntary euthanasia. Fam Med. 2000;32(4):261–6.
Prendergast TJ, Luce JM. Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Respir Crit Care Med. 1997;155(1):15–20.
Doyal L, Wilsher D. Withholding and withdrawing life sustaining treatment from elderly people: towards formal guidelines. BMJ (Clin Res Ed). 1994;308(6945):1689–92.
Solomon MZ, O'Donnell L, Jennings B, et al. Decisions near the end of life: professional views on life-sustaining treatments. Am J Public Health. 1993;83(1):14–23.
Consensus report on the ethics of foregoing life-sustaining treatments in the critically ill. Task Force on Ethics of the Society of Critical Care Medicine. Crit Care Med. Dec 1990;18(12):1435-1439.
Withholding and withdrawing life-sustaining therapy. Ann Intern Med. Sep 15 1991;115(6):478-485.
Truog RD, Campbell ML, Curtis JR, et al. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med. 2008;36(3):953–63.
Hawryluck LA, Harvey WR, Lemieux-Charles L, Singer PA. Consensus guidelines on analgesia and sedation in dying intensive care unit patients. BMC Med Ethics. 2002;3:E3.
Approaching death: improving care at the end of life—a report of the Institute of Medicine. Health Serv Res. Apr 1998;33(1):1-3.
Rubenfeld GD, Curtis JR. Beyond ethical dilemmas: improving the quality of end-of-life care in the intensive care unit. Crit Care. 2003;7(1):11–2.
NIH State-of-the-Science Conference Statement on improving end-of-life care. NIH Consens State Sci Statements. Dec 6-8 2004;21(3):1-26.
Field MJ, Cassel CK. Approaching death: improving care at the end of life. Health Prog. 2011;92(1):25.
Prendergast TJ, Puntillo KA. Withdrawal of life support: intensive caring at the end of life. JAMA. 2002;288(21):2732–40.
Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med. 2003;18(9):685–95.
Fischer SM, Gozansky WS, Kutner JS, Chomiak A, Kramer A. Palliative care education: an intervention to improve medical residents' knowledge and attitudes. J Palliat Med. 2003;6(3):391–9.
Gorman TE, Ahern SP, Wiseman J, Skrobik Y. Residents' end-of-life decision making with adult hospitalized patients: a review of the literature. Acad Med. 2005;80(7):622–33.
Schroder C, Heyland D, Jiang X, Rocker G, Dodek P. Educating medical residents in end-of-life care: insights from a multicenter survey. J Palliat Med. 2009;12(5):459–70.
Ogle KS, Mavis B, Thomason C. Learning to provide end-of-life care: postgraduate medical training programs in Michigan. J Palliat Med. 2005;8(5):987–97.
Mullan PB, Weissman DE, Ambuel B, von Gunten C. End-of-life care education in internal medicine residency programs: an interinstitutional study. J Palliat Med. 2002;5(4):487–96.
Ury WA, Rahn M, Tolentino V, et al. Can a pain management and palliative care curriculum improve the opioid prescribing practices of medical residents? J Gen Intern Med. 2002;17(8):625–31.
Weissman DE, Ambuel B, von Gunten CF, et al. Outcomes from a national multispecialty palliative care curriculum development project. J Palliat Med. 2007;10(2):408–19.
Weissman DE, Mullan PB, Ambuel B, von Gunten C. End-of-life curriculum reform: outcomes and impact in a follow-up study of internal medicine residency programs. J Palliat Med. 2002;5(4):497–506.
Minor S, Schroder C, Heyland D. Using the intensive care unit to teach end-of-life skills to rotating junior residents. Am J Surg. 2009;197(6):814–9.
Fins JJ, Nilson EG. An approach to educating residents about palliative care and clinical ethics. Acad Med. 2000;75(6):662–5.
Stillman P, Swanson D, Regan MB, et al. Assessment of clinical skills of residents utilizing standardized patients. A follow-up study and recommendations for application. Ann Intern Med. 1991;114(5):393–401.
Stillman PL, Swanson DB. Ensuring the clinical competence of medical school graduates through standardized patients. Arch Intern Med. 1987;147(6):1049–52.
ACKNOWLEDGMENTS
We thank Pete Charpentier and Katy Araujo for their capable assistance with data entry and analysis. The research reported in this manuscript was supported by the James G. Hirsch, MD, Endowed Medical Student Research Fellowship. This sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Conflicts of interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomas, J.M., O’Leary, J.R. & Fried, T.R. A Comparison of the Willingness of Resident and Attending Physicians to Comply with the Requests of Patients at the End of Life. J GEN INTERN MED 29, 1048–1054 (2014). https://doi.org/10.1007/s11606-014-2830-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-2830-0