Abstract
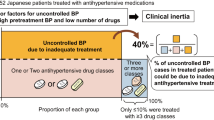
The Hypertension in the Very Elderly trial (HYVET), demonstrated the benefit of antihypertensive treatment in patients ⩾80 years. However, patients in this age group are at increased risk of drug interactions and adverse effects. We conducted a retrospective cohort study, in hypertensive patients aged ⩾80 years, to determine whether it is possible to follow the HYVET guidelines in an everyday clinical setting. We identified 100 patients aged ⩾80 years referred to the Hypertension Clinic, University Hospital Birmingham, over a 10-year period. Most patients were referred to the clinic because of poorly controlled blood pressure despite treatment and all had 24 h ambulatory blood pressure monitoring (ABPM) as part of their assessment. All patients tolerated ABPM, and a ‘white coat’ effect was demonstrated in 33 patients. In 64 out of 100 patients (57 on treatment), the ABPM confirmed poor blood pressure control. Despite this, 26 of these patients had an antihypertensive either stopped (15), and /or reduced (3) or left unchanged (9) at clinic because of documented adverse drug reactions (ADRs). In 36 out of 100 patients, no additional antihypertensive therapy was needed because the blood pressure was either well-controlled on treatment (28), over-treated (4), or normotensive with a white coat effect (4). Despite this, antihypertensive agents were either stopped (10), and or reduced (5) because of ADRs in half the patients (14) from the well-controlled group. In conclusion, 40% patients had documented ADRs overall which limited further intervention, suggesting that implementation of the HYVET recommendations in clinical practice may be difficult.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Dunnell K . The changing demographic picture of the UK: national statistician's annual article on the population. Popul Trends 2007; 130: 9–21.
Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens 2004; 18 (3): 139–185.
Gueyffier F, Bulpitt C, Boissel JP, Schron E, Ekbom T, Fagard R et al. Antihypertensive drugs in very old people: a subgroup meta-analysis of randomised controlled trials. INDANA Group. Lancet 1999; 353 (9155): 793–796.
Oates DJ, Berlowitz DR, Glickman ME, Silliman RA, Borzecki AM . Blood pressure and survival in the oldest old. J Am Geriatr Soc 2007; 55 (3): 383–388.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358 (18): 1887–1898.
Kostis JB . Treating hypertension in the very old. N Engl J Med 2008; 358 (18): 1958–1960.
Milton JC, Hill-Smith I, Jackson SH . Prescribing for older people. BMJ 2008; 336 (7644): 606–609.
Mallet L, Spinewine A, Huang A . The challenge of managing drug interactions in elderly people. Lancet 2007; 370 (9582): 185–191.
Williamson J, Chopin JM . Adverse reactions to prescribed drugs in the elderly: a multicentre investigation. Age Ageing 1980; 9: 73–80.
Mann R, Andrews E . Pharmacovigilance, 2nd edn. John Wiley and sons Ltd: England, UK, 2007.
Mets TF . Drug-induced orthostatic hypotension in older patients. Drugs Ageing 1995; 6 (3): 219–228.
Salzman C . Clinical Geriatric Psychopharmacology, 4th edn. Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005.
Morrow D, Leirer V, Sheikh J . Adherence and medication instructions review and recommendations. J Am Geriatr Soc 1988; 36 (12): 1147–1160.
Chavanu K, Merkel J, Quan AM . Role of ambulatory blood pressure monitoring in the management of hypertension. Am J Health Syst Pharm 2008; 65 (3): 209–218.
Wing LM, Brown MA, Beilin LJ, Ryan P, Reid CM . ANBP2 Management Committee and Investigators. Second Australian National Blood Pressure Study. J Hypertens 2002; 20 (4): 639–644.
Pinto E, Bulpitt C, Beckett N, Peters R, Staessen JA, Rajkumar C . Rationale and methodology of monitoring ambulatory blood pressure and arterial compliance in the Hypertension in the Very Elderly Trial. Blood Press Monit 2006; 11 (1): 3–8.
Acknowledgements
We would like to thank the University of Birmingham for sponsoring this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Butt, T., Branch, R., Beesley, L. et al. Managing hypertension in the very elderly: effect of adverse drug reactions (ADRs) on achieving targets. J Hum Hypertens 24, 514–518 (2010). https://doi.org/10.1038/jhh.2009.116
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2009.116
Keywords
This article is cited by
-
Antihypertensive-related adverse drug reactions among older hospitalized adults
International Journal of Clinical Pharmacy (2018)
-
Prevalence, prescribing and barriers to effective management of hypertension in older populations: a narrative review
Journal of Pharmaceutical Policy and Practice (2015)
-
Impact of Hospitalization on Antihypertensive Pharmacotherapy among Older Persons
Drugs - Real World Outcomes (2015)
-
Hypertension therapy in the older adults—do we know the answers to all the questions? The status after publication of the ACCF/AHA 2011 expert consensus document on hypertension in the elderly
Journal of Human Hypertension (2012)
-
Hypertension in the Elderly: What Is the Goal Blood Pressure Target and How Can This Be Attained?
Current Hypertension Reports (2010)