Abstract
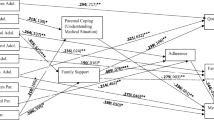
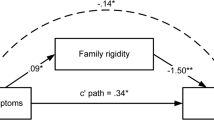
Background: Diabetes is a common disease in pediatric populations. Family functioning has been related to child adaptation to diabetes. Purpose: To determine the impact of family factors on diabetes, particularly the influence of family support and family environment on adherence to treatment, quality of life, and metabolic control in Portuguese adolescents with type 1 diabetes, taking in consideration age, sex, duration of disease, and social class. Method: This study used a cross-sectional design. A sample of 157 Portuguese diabetic patients filled disease-specific measures on adherence and quality of life and family functioning measures. Hypotheses were that family support and an organized family environment (high cohesion and low conflict) would be positively associated with better adherence, metabolic control, and quality of life. Results: This study’s results confirmed that adherence was predicted by family support for females and lower-class patients while metabolic control was predicted by family conflict for upper-class patients. Quality of life was predicted by lack of family conflict and family social support for both males and females as well as lower-class patients. Conclusion: The results highlight the importance of studying family variables in adolescents’ diabetes care within the wider cultural factors affecting the patient.
Similar content being viewed by others
References
Alemzadeh, R., & Wyatt, D. T. (2004). Diabetes mellitus in children. In Nelson Textbook of Pediatrics, 17th ed. Behrman, R. E., Kliegman, R. M., and Jenson, H. B. (Eds), (pp. 1947–1972). Philadelphia: W.B. Saunders Co.
Almeida, P., & Pereira, M. G. (2003). Self-report questionnaire on adherence. Experimental version. Department of Psychology, Braga, Portugal: University of Minho.
Anderson, B. J., Brackett, J., Finkelstein, D., & Laffel, L. (1997). Parental involvement in diabetes management tasks: Relationship to blood glucose monitoring and metabolic control in adolescents with insulin-dependent diabetes-mellitus. The Journal of Pediatrics, 130(2), 257–265.
Barakat, L. P., & Kazak, A. E. (1999). Family issues. In R. T. Brown (Ed.), Cognitive aspects of chronic illness in children. New York: Guilford Press.
Cohen, D. M., Lumley, M. A., Naar-King, S., Partridge, T., & Cakan, N. (2004). Child behavior problems and family functioning as predictors of adherence and glycemic control in economically disadvantaged children with type 1 diabetes: A prospective study. Journal of Pediatric Psychology, 29(3), 171–184.
Diabetes Control and Complications Trial Research Group (DCCT). (1993). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine, 329, 977–986.
Dickenson, L. M., Ye, X., Sack, J., & Hueston, W. (2003). General quality of life in youth with type 1 diabetes: Relationship to patient management and diabetes-specific family conflict. Diabetes Care, 26, 3067–3073.
Donnelly, L. A., Morris, A. D., & Evans, J. M. (2007). Adherence to insulin and its association with glycemic control in patients with type 2 diabetes. Quarterly Journal of Medicine, 100(6), 345–350.
Drotar, D. (1997). Relating parent and family functioning to the psychological adjustment of children with chronic conditions: What have we learned? What do we need to know? Journal of Pediatric Psychology, 22(2), 159–166.
Garay-Sevilla, M. E., Nava, L. E., Malacara, J. M., Huerta, R., de Leon, J. D., Mena, A., et al. (1995). Adherence to treatment and social support in patients with NIDDM. Journal of Diabetics Complications, 9(2), 81–86.
Gillibrand, R. A., & Stevenson, J. (in press). The role of partner relationships in the young person’s adherence to the diabetes self-care regime. International Journal of Behavioral Medicine, (Pages: under review).
Glasgow, R. (1991). Compliance to diabetes Regimens: Conceptualization, complexity and determinants. In J. A. Cramer & Spilker: Patient Compliance in Medical Practice and Clinical Trial (pp. 123–137). Raven Press, Lda. New York.
Glasgow, R., McCaul, K. D., & Schaffer, L.C. (1987). Self care behaviours and glycemic Control in type 1 Diabetes. Journal of Chronic Disease, 40, 65–77.
Graffar, M. (1956). Une methode de classification socialle-échantillions de population. Courrier, 6, 445–449.
Grey, M., Boland, E., Yu, C., Sullivan-Bollyai, A., & Tamborlane, W. V. (1998). Personal and family factors associated with quality of life in adolescents with diabetes. Diabetes Care, 212(6), 909–914.
Guttmann-Bauman, I., Flaherty, B. P., Strugger, M., & McEvoy, R. C.(1998). Metabolic control and quality of life self-assessment in adolescents with IDDM. Diabetes Care, 21(6), 915–918.
Hamlet, K. W., Pellegrini, D. S., & Katz, K. S. (1992). Childhood chronic illness as a family stressor. Journal of Pediatric Psychology, 17, 33–47.
Hanson, C., Cigrang, J., Harris, M., Carle, D., Relyea, G., & Burghen, G. (1989b). Coping styles in youths with insulin-dependent diabetes mellitus. Journal of Consulting and Clinical Psychology, 57, 644–651.
Hanson, C. L., Henggeler, S. W., & Burghen, G. A. (1987). Social competence and parental support as mediators of the link between stress and metabolic control in adolescents with insulin-dependent diabetes mellitus. Journalof Consulting and Clinical Psychology, 55, 529–533.
Hanson, C., Henggeler, S. W., Burghen, G., & Moore, M. (1989a). Family system variable and the health status of adolescents with insulin-dependent diabetes mellitus.Health Psychology, 8(2), 239–253.
Hoey, H., Aanslot, H.-J., Chiarelli, F., Daneman, D., Danne, T., Dorchy, H., et al. (2001). Good metabolic control is associated with better quality of life in 2101 adolescents with type 1 diabetes. Diabetes Care, 24(11), 1923–1928.
Horner, S. D. (1997). Uncertainty in mothers’ care for their ill children. Journal of Advanced Nursing, 26(4), 658–663.
Injersoll, G., & Marrero, D. (1991). A modified quality of life measure for youths: Psychometric properties. The Diabetes Educator, 17(2), 114–118.
ISPAD & IDF (2000). ISPAD consensus guidelines for the management of type 1 diabetes mellitus in children and adolescents. Medical Forum International, The Netherlands.
ISPAD, IDF, & WHO (St. Vincent & Kos Declarations). (1995). Consensus guidelines for the management of insulin-dependent (type 1) diabetes mellitus (IDDM). In Childhood and adolescence. London: Freund.
Jacobson, A. M., Hauser, S. T., Lavori, P., Wolfsdorf, J. I., Herskowitz, R. D., Miley, J. E.,et al. (1990). Adherence among children and adolescents with insulin-dependent diabetes mellitus over a four-year longitudinal follow-up. I. The influence of patient coping and adjustment. Journal of Pediatric Psychology, 15(4), 511–526.
Johnson, S. B. (1994). Health behavior and health status: Concepts, methods and applications. Journal of Pediatric Psychology, 19(2), 129–142.
Johnson, S. B., Freund, A., Silverstein, J., Hansen, C., & Malone, J. (1990). Adherence-health status relationships in childhood diabetes. Health Psychology, 9, 606–631.
Kilo, C., & Williamson, J. R. (1987). Diabetes: The facts that let you regain control over your life. New York: Wiley.
Kovacs, M., Brent, D., Steinberg, T. F., Paulauskas, S., & Reid, J. (1986). Children’s self-reports of psychologic adjustment and coping strategies during the first years of insulin-dependent diabetes mellitus. Diabetes Care, 9, 472–479.
Krapek, K., King, K., Warren, S., George, K., Caputo, D., Mihe-lich, K., et al. (2004). Medication adherence and associated hemoglobin A1c in type 2 diabetes. The Annals of Pharma-cotherapy, 38(9), 1357–1362.
La Greca, A. M., & Thomson, K. M. (1998). Family and friend support for adolescents with diabetes. Análise Psicológica, 1 (XVI), 101–113.
La Greca, A. M., Auslander, W. F, Greco, P., Spetter, D., Fisher, E. B., & Santiago, J. V. (1995). I get by a little help from my family and friends: Adolescent’s support for diabetes care. Journal of Pediatric Psychology, 20, 449–476.
Leonard, B. J., Garwick, A., & Adwan, J. Z. (2005). Adolescent’s perceptions of parental roles and involvement in diabetes management. Journal of Pediatric Nursing, 20(6), 405–414.
Leonard, B. J., Savik, K., Plumbo, P. M., & Christensen, R. (2002). Psychosocial factors associated with levels of metabolic control in youth with type 1 diabetes. Journal of Pediatric Nursing, 17(1), 28–37.
Lewin, A., Heidgerken, A., Geffken, G., Williams, L., Storch, E., Gelfand, K., & Silverstein, J. (2006). The relation between family factors and metabolic control: The role of diabetes adherence. Journal of Pediatric Psychology, 31(2), 174–183.
Martin, M. T., Miller-Johnson, S., Kitzmann, K. M., & Emery, R. E. (1998). Parent-child relationships and insulin dependent diabetes mellitus: Observational ratings of clinically relevant dimensions. Journal of Family Psychology, 12(1), 102–111.
McCubbin, M. A., & McCubbin, H. I. (1993). Families coping with illness: The resilience model of family stress, adjustment, and adaptation. In C. B. Danielson, B. Hamel-Bissell, & P. Winstead-Fry (Eds.), Families, health, and illness: Perspectives on coping and intervention. St. Louis, MO: Mosby-Year Book.
Mckelvey, J., Walter, D., North, A. J., Marks, J. F., Schreiner, B., Travis, L. B., et al. (1993). Reliability and validity of the Diabetes Family Behavior Scale (DFBS). The Diabetes Educator, 19(2), 125–132.
Moos, R. H., & Moos, B. S. (1986). Family environment scale manual. Palo Alto, CA: Consulting Psychologists Press.
Palardy, N., Greening, L., Ott, J., Holderby, A., & Atchinson, J. (1998). Adolescents’ health attitudes and adherence to treatment for insulin-dependent diabetes mellitus. Developmental and Behavioral Pediatrics, 19(1), 31–37.
Pinar, R., Erslanoglu, I., Isguven P., Cizmeci F., & Gunoz H. (2003). Self-efficacy and its interrelation with family environment and metabolic control in Turkish adolescents with type 1 diabetes. Pediatric Diabetes, 4(4), 168–173.
Santiago, J. V. (1984). Effect of treatment on the long term complications of IDDM. Behavioral Medicine Update, 6,(1), 26–31.
Sarafino, E. P. (1990). Health psychology: Byopsicossocial Interactions. New York, John Wiley & Sons.
Seiffe-Krenke, I. (1998). Psychological adjustment of adolescents with diabetes: Functional or dysfunctional for metabolic control? Journal of Pediatric Psychology, 23(5), 313–322.
Silver, E. J., Stein, R. E. K., & Dadds, M. R. (1996). Moderating effects of family structure on the relationship between physical and mental health in urban children with chronic illness. Journal of Pediatric Psychology, 21(1), 43–56.
Sperling, A. M. (1996). Diabetes mellitus. In W. E. Nelson, R. M. Behrman, & A. M. Arvin (Ed.), Nelson textbook of pediatrics (15th ed.). Philadelphia: WB Sanders.
Toobert, D. J., & Galasgow, R. (1996). Assessing diabetes self-management: The summary of diabetes self care activities questionnaire. In C. Bradley (Ed.). Handbook of psychology and diabetes. London: Harwood Academic.
Warren, L., & Hixenbaugh, P. (1996). The role of health beliefs and locus of control on regimen adherence from a life-span perspective. Proceedings of the British Psychological Society, 5, 17.
Williams, G. C., Freedman, Z. R., & Deci, E. L. (1998). Supporting Autonomy to motivate patients with diabetes for glucose control. Diabetes Care, 21(10), 1644–1651.
Wilson, W., Ary, D. V., Biglan, A., Glasgow, R. E., Toober, D. J., & Campbell, D. R. (1986). Psychosocial predictors of self-care behaviors (compliance) and glycemic control in non-insulin dependent diabetes mellitus. Diabetes Care, 9, 614–622.
Wing, R. R., Nowalk, M. P., & Guare, J. C. (1988). Diabetes mellitus. In E. A. Bleckman & K. D. Bownell (Eds.), Handbook of behavioral medicine for women. New York: Pergamon.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Graça Pereira, M., Berg-Cross, L., Almeida, P. et al. Impact of family environment and support on adherence, metabolic control, and quality of life in adolescents with diabetes. Int. J. Behav. Med. 15, 187–193 (2008). https://doi.org/10.1080/10705500802222436
Issue Date:
DOI: https://doi.org/10.1080/10705500802222436