Abstract
BACKGROUND: Guidelines recommend tight control of hemoglobin Alc (HbAlc), low-density lipoprotein cholesterol (LDL-C), and blood pressure (BP) for patients with diabetes. The degree to which these intermediate outcomes are simultaneously controlled has not been extensively described.
OBJECTIVE: Describe the degree of simultaneous control of HbAlc, LDL-C, and BP among Veterans Affairs (VA) diabetes patients defined by both VA and American Diabetes Association (ADA) guidelines.
DESIGN: Cross-sectional cohort.
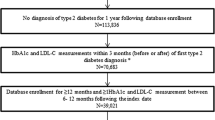
PATIENTS: Eighty-thousand two hundred and seven VA diabetes patients receiving care between October 1999 and September 2000.
MEASURMENTS: We defined simultaneous control of outcomes using 1997 VA Guidelines (in place in 2000) (HbAlc<9.0%; LDL-C<130 mg/dL; systolic BP<140mmHg; and diastolic BP<90mmHg) and 2004 ADA guidelines (HbAlc<7.0%; LDL-C<100 mg/dL; systolic BP<130 mmHg; and diastolic BP<80 mmHg). A patient is considered to have simultaneous control of the intermediate outcomes for a given definition if the average of measurements for each outcome was below the defined threshold during the study period.
RESULTS: Using VA guidelines, 31% of patients had simultaneous control. Control levels of individual outcomes were: HbAlc (82%), LDL-C (77%), and BP (48%). Using ADA guidelines, 4% had simultaneous control. Control levels of individual outcomes were: HbAlc (36%), LDL-C (41%), and BP (23%). Associations between individual risk factors were weak. There was a modest association between LDL-C control and control of HbAlc (odds ratio [OR] 1.51; 95% confidence interval [CI] 1.44, 1.58). The association between LDL-C and BP control was clinically small (1.26: 1.21, 1.31), and there was an extremely small association between BP and HbAlc control (0.95; 0.92, 0.99). Logistic regression modeling indicates greater body mass index, African American or Hispanic race-ethnicity, and female gender were negatively associated with simultaneous control.
CONCLUSION: While the proportion of patients who achieved minimal levels of control of HbAlc and LDL-C was high, these data indicate a low level of simultaneous control of HbAlc, LDL-C, and BP among patients with diabetes.
Similar content being viewed by others
References
Khaw K-T, Wareham N, Bingham S, Luben R, Welch A, Day N. Association of hemoglobin Alc with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med. 2004;141:413–20.
Selvin E, Marinoppulos S, Berkenblit G, et al. Meta-analysis. Glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141:421–31.
Stratton IM, Adler AI, Neil HAW, et al. Association of glycemia with macrovascular and microvascular conditions of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–12.
Vijan S, Hayward RA. Pharmacologic lipid-lowering therapy in type 2 diabetes mellitus: background paper for the American College of Physicians. Ann Intern Med. 2004;140:650–8.
Adler AI, Stratton IM, Neil HAW, et al. Association of systolic blood pressure with macrovascular and microvascular complication of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–9.
Snow V, Weiss KB, Mottur-Pilson C, for the Clinical Efficacy Assessment Subcommittee of the American College of Physicians. The evidence base for tight blood pressure control in the management of type 2 diabetes. Ann Intern Med. 2003;138:587–92.
Bruno G, Cavallo-Perin P, Bargero G, Borra M, D’Errico N, Pagano G. Glycaemic control and cardiovascular risk factors in type 2 diabetes: a population-based study. Diabetes Med. 1998;15:304–7.
Harris MI. Health care and health status and outcomes for patients with type 2 diabetes. Diabetes Care. 2000;23:754–8.
Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KMV. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–74.
Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291:335–42.
Smith NL, Savage PJ, Heckbert SR, et al. Glucose, blood pressure, and lipid control in older people with and without diabetes mellitus: the Cardiovascular Health Study. J Am Geriatr Soc. 2002;50:416–23.
Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. Racial disparities in diabetes care processes, outcomes, and treatment intensity. Med Care. 2003;41:1221–32.
Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the Veterans Affairs health care system and commercial managed care: the TRIAD Study. Ann Intern Med. 2004;141:272–81.
Smith NL, Chen L, Au DH, McDonell M, Fihn SD. Cardiovascular risk factor control among veterans with diabetes. Diabetes Care. 2004;27:B33–8.
Beaton SJ, Nag SS, Gunter MJ, Gleeson JM, Saigan SS, Alexander CM. Adequacy of glycemic, lipid, and blood pressure management for patients with diabetes in a managed care setting. Diabetes Care. 2004;27:694–8.
Bouma M, Dekker JH, van Eijk JThM, Schellevis FG, Kriegsman DMW, Heine RJ. Metabolic control and morbidity of type 2 diabetic patients in a general practice network. Fam Pract. 1999;16:402–6.
Kell SH, Drass J, Bausell B, Thomas KA, Osborn MA, Gohdes D. Measures of disease control in Medicare beneficiaries with diabetes mellitus. J Am Geriatr Soc. 1999;47:417–22.
Kim C, Williamson DF, Mangione CM, et al. Managed care organization and the quality of diabetes care. Diabetes Care. 2004;27:1529–34.
McFarlane SI, Jacober SJ, Winer N, et al. Control of cardiovascular risk factors in patients with diabetes and hypertension at urban academic medical centers. Diabetes Care. 2002;25:718–23.
Porterfield DS, Kinsinger L. Quality of care for uninsured patients with diabetes in a rural area. Diabetes Care. 2002;25:319–23.
Putzer GJ, Ramirez AM, Sneed K, Brownlee HJ, Roetzheim RG, Campbell RJ. Prevalence of patients with type 2 diabetes mellitus reaching the American Diabetes Association’s target guidelines in a university primary care setting. South Med J. 2004;97:145–8.
Wandell PE, Gafvels C. Metabolic controland quality of data in medical records for subjects with type 2 diabetes in Swedish primary care: improvement between 1995 and 2001. Scand J Prim Health Care. 2002;20:230–5.
Narayan KMV, Benjamin E, Gregg EW, Norris SL, Engelgau MM. Diabetes translation research: where are we and where do we want to be. Ann Intern Med. 2004;140:958–63.
Renders CM, Calk GD, Griffin SJ, et al. Interventions to improve the management of diabetes in primary care, outpatient, and community settings, a systematic review. Diabetes Care. 2001;24:1821–33.
Healthcare Analysis and Information Group, Quality Enhancement Research Initiative-Diabetes Mellitus. VA Diabetes Registry and Dataset [fact sheet], VA Ann Arbor QUERI-DM Research Coordinating Center, Ann Arbor, MI, November 22, 2002.
Hawley G: VIReC Briefing. HAIG Diabetes Projects [presentation available on the World Wide Web]. June 20, 2001. Available at: http://www.hsrd.ann-arbor.med.va.gov/queri/HAIGdiabetes2001.pdf. Accessed March 10, 2005.
Maynard C, Chapko MK. Data resources in the Department of Veterans Affairs. Diabetes Care. 2004;27:B22–6.
Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major U.S. mortality databases. Ann Epidemiol. 2002;12:462–8.
Agency for Healthcare Research and Quality. Clinical Classification Software (CCS), 2003, Software and User’s Guide; February, 2003. Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed March 10, 2005.
Rosen AK, Trivedi P, Amuan M, Montez M. The Johns Hopkins Adjusted Clinical Groups (ACGs) Case-Mix System: a risk-adjustment methodology currently available at the VA Austin Automation Center. VIReC Insights, 2003;4:1–10. Available at: http://www.virec.research.med.va.gov/References/VirecInsights/Insights-v04nl.pdf. Accessed March 10, 2005.
Jackson GL, Yano EM, Edelman D, et al. Veterans affairs primary care organizational characteristics associated with better diabetes control. Am J Manage Care. 2005;11:225–50.
Leinung MC, Gianoukakis AG, Lee DW, Jeronis SL, Desemone J. Comparison of diabetes care provided by and endocrinology clinic and a primary-care clinic. Endocrine Pract. 2000;6:361–6.
Clark MJ Jr,Sterrett JJ, Carson DS. Diabetes guidelines. A summary comparison of the recommendations of the American Diabetes Association, Veterans Health Administration, and American Association of Clinical Endocrinologists. Clin Ther. 2000;22:899–910.
American Diabetes Association. Clinical practice recommendations 2004. Diabetes Care. 2004;27:S1–150.
SAS Institute Inc. SAS [computer program] Version 9.1. Cary, NC: SAS Institute Inc.: 2003.
Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56:645–6.
StataCorp. Intercooled Stata [computer program] Version 8.2. College Station, TX: SAS Institute Inc.; 2004.
Asch SM, McGlynn EA, Hogan MM, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Intern Med. 2004;141:938–45.
Clark NM. Management of chronic disease by patients. Ann Rev Public Health. 2003;24:289–313.
Alexander SC, Sleath B, Golin CE, Kalinowski CT. Provider-patient communication and treatment adherence. In: Bosworth HB, Oddone EZ, Weinberger M, eds. Patient Treatment Adherence: Concepts, Interventions, and Measurement. Mahwah, NJ: Lawrence Erlbaum Associates; 2005:329–72.
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52.
Cook CB, Ziemer DC, El-Kebbi IM, et al. Diabetes in urban African-Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes. Diabetes Care. 1999;22:1494–500.
Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34.
Ziemer DC, Miller CD, Rhee MK, et al. Clinical inertia contributes to poor diabetes control in a primary care setting. Diabetes Educ. 2005;31:564–71.
Johnson CL, Rifkind BM, Sempos CT, et al. Declining serum total cholesterol levels, The National Health and Nutrition Examination Surveys. JAMA. 1993;269:3002–8.
Joffres MR, Hamet P, MacLean DR, L’italien GJ, Fodor G. Distribution of blood pressure and hypertension in Canada and the United States. Am J Hypertens. 2001;14:1099–105.
Dagogo-Jack S. Ethnic disparities in type 2 diabetes: pathophysiology and implications for prevention and management. J Natl Med Assoc. 2003;95:774, 779–89.
Acton KJ, Preston S, Rith-Najarian S. Clinical hypertension in Native Americans: a comparison of 1987 and 1992 rates from ambulatory care data. Public Health Rep. 1996;111:33–6.
Welty TK, Lee ET, Yeh J, et al. Cardiovascular disease risk factors among American Indians: the Strong Heart Study. Am J Epidemiol. 1995;142:269–87.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation. 2002;106:3143–421.
Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manage Care. 2004;10:828–36.
Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–44.
Bosworth HB, Oddone EZ. A model of psychosocial and cultural antecedents of blood pressure control. J Natl Med Assoc. 2002;94:236–48.
Author information
Authors and Affiliations
Additional information
He is currently a Veterans Affairs Health Services Research & Development Merit Review Entry Program awardee (VA grant MRP 05-312). Dr. Weinberger is a VA Health Services Research & Development Senior Career Scientist awardee. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Rights and permissions
About this article
Cite this article
Jackson, G.L., Edelman, D. & Weinberger, M. Simultaneous control of intermediate diabetes outcomes among veterans affairs primary care patients. J GEN INTERN MED 21, 1050–1056 (2006). https://doi.org/10.1111/j.1525-1497.2006.00519.x
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2006.00519.x