ABSTRACT
BACKGROUND
A high proportion of the US primary care workforce reports burnout, which is associated with negative consequences for clinicians and patients. Many protective factors from burnout are characteristics of patient-centered medical home (PCMH) models, though even positive organizational transformation is often stressful. The existing literature on the effects of PCMH on burnout is limited, with most findings based on small-scale demonstration projects with data collected only among physicians, and the results are mixed.
OBJECTIVE
To determine if components of PCMH related to team-based care were associated with lower burnout among primary care team members participating in a national medical home transformation, the VA Patient Aligned Care Team (PACT).
DESIGN
Web-based, cross-sectional survey and administrative data from May 2012.
PARTICIPANTS
A total of 4,539 VA primary care personnel from 588 VA primary care clinics.
MAIN MEASURES
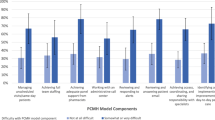
The dependent variable was burnout, and the independent variables were measures of team-based care: team functioning, time spent in huddles, team staffing, delegation of clinical responsibilities, working to top of competency, and collective self-efficacy. We also included administrative measures of workload and patient comorbidity.
KEY RESULTS
Overall, 39 % of respondents reported burnout. Participatory decision making (OR 0.65, 95 % CI 0.57, 0.74) and having a fully staffed PACT (OR 0.79, 95 % CI 0.68, 0.93) were associated with lower burnout, while being assigned to a PACT (OR 1.46, 95 % CI 1.11, 1.93), spending time on work someone with less training could do (OR 1.29, 95 % CI 1.07, 1.57) and a stressful, fast-moving work environment (OR 4.33, 95 % CI 3.78, 4.96) were associated with higher burnout. Longer tenure and occupation were also correlated with burnout.
CONCLUSIONS
Lower burnout may be achieved by medical home models that are appropriately staffed, emphasize participatory decision making, and increase the proportion of time team members spend working to the top of their competency level.
Similar content being viewed by others
BACKGROUND
Employee burnout is characterized by emotional exhaustion, depersonalization, and a low sense of personal accomplishment.1,2 Burned-out employees are more likely to leave their jobs,1,3–7 take sick leave, and suffer from relationship problems and depression.8–10 Clinician burnout is associated with worse patient safety11–15 and satisfaction.16–18 By some estimates, burnout affects nearly half of all US nurses and physicians.1,19
There are many contributors to burnout. Employees who experience long work hours, excessive clinical workloads, a chaotic work environment, or discord among fellow staff are more likely to have burnout.5,8,10,20 Conversely, those who report a greater institutional emphasis on quality of care, team cohesiveness and communication are less likely to report burnout.5 Adequate staffing levels, equitable distribution of clinical work, as well as opportunities for skill development, may be protective.2,21 Likewise, a sense of control over work schedule and environment, autonomy, and participation in organizational decision making are associated with lower burnout.20 Many of these factors are characteristics of patient-centered medical home (PCMH) models, which emphasize coordination of care, more efficient distribution of clinical tasks, and a collaborative work environment.
However, there has been limited research on the association of PCMH implementation with burnout or job satisfaction.22,23 In the Group Health Cooperative medical home pilot, characterized by smaller panel sizes and greater visit durations, Reid and colleagues reported a 1-year decrease in provider burnout from 30 % to 10 %, while it did not change at control clinics. These differences in burnout persisted through the second year of their PCMH.24,25 They attributed this decrease to reduced panel sizes, greater time with patients, and a more supportive work environment.25 Hochman and colleagues likewise found that implementation of PCMH in a single resident physician clinic was associated with improved job satisfaction.26 However, Nutting and colleagues reported change fatigue, including burnout and turnover, among participants in the National Demonstration Project,27 and Lewis and colleagues found greater PCMH characteristics associated with high staff morale, but also higher provider burnout, among 65 safety-net clinics in a 2010 survey.28 Moreover, organizational research has previously found workplace change—particularly frequent change or multiple changes—associated with greater burnout.29,30 In addition to offering conflicting findings, the existing literature on PCMH implementation and burnout is limited by small sample sizes, generally restricted to PCMH demonstration sites, and a focus almost exclusively on the physician experience.22,23 Overall, it remains unclear what effect broad-based PCMH implementation will have on a primary care workforce, including nurses and other staff, that is already exhibiting high levels of stress.
In April 2010, the Veteran’s Health Administration (VHA) launched the Patient Aligned Care Team (PACT) initiative to implement a PCMH model in VHA primary care nationally.31 PACT, described in detail elsewhere,31,32 emphasized team-based care to improve clinical continuity, coordination and patient-centeredness. The teams, or PACTs, comprised a primary care provider (PCP) (i.e., a physician, nurse practitioner or a physician assistant), a nurse care manager, a clinical associate (e.g., LPN, medical assistant) and an administrative clerk. The VHA provided resources to support PACT implementation, such as funding to expand the staffing model to 3.0 Full-time equivalent (FTE) support staff for each PCP. There was an emphasis on communication and participatory decision making to develop well-functioning teams. PACTs were encouraged to use brief daily meetings or “huddles” to better coordinate work. There was education about different team roles, notably for the nurse care manager, who promotes wellness and self-care, and conducts proactive outreach to patients, including electronic and telephone contacts. Early findings suggest substantial progress in implementing the PACT model,32,33 with increases in the use of telephone and electronic encounters, and proactive follow-up after hospital admissions, as well as reductions in hospitalizations for ambulatory sensitive conditions.32,34 However, one-third of primary care employees report signs of burnout,33 and there appear to be strong temporal trends in declining job satisfaction and workplace climate among VA PCPs.35 The stress of a large-scale change could be contributing to burnout among employees, or conversely, this team-based care model, which has characteristics associated with lower burnout in other settings,2,5,8,10,20,21,36–38 could be protective of burnout.
Our aim was to test the association of specific PACT elements with burnout among primary care employees approximately 2 years into a medical home transformation that is still underway, in order to better understand how broad-based implementation of a team-based PCMH model affects primary care employees.
METHODS
We conducted a cross-sectional, web-based survey in May–June 2012. Survey links were distributed via e-mail through clinical leadership in Primary Care and Nursing. Clinical leaders were asked to distribute the surveys to all staff that worked in primary care. Surveys were anonymous, with only clinic identifiers. The survey was approved by national union representatives.
With the exception of two of the 21 networks, all VA primary care team members (PCPs, nurses care managers, clinical associates and administrative clerks) employed by VA in summer 2012 were eligible to participate. The two networks that did not participate were demonstration sites that fielded similar but more in-depth surveys not reported here.
MAIN MEASURES
The dependent variable was burnout, measured using a single-item, 5-point measure39 used for the Physician Worklife Study (PWS).40,41 A score of 3 or higher indicated signs of burnout.41 In sensitivity analyses, we also analyzed the PWS burnout measure as an ordinal value, and a 3-item version of the Maslach Burnout Inventory (MBI) Emotional Exhaustion scale.42 In the study sample, the PWS had a sensitivity of 78 % and specificity of 88 % for detecting burnout as indicated by the MBI, with an area under the curve (AUC) of 0.91.43
We assessed implementation of PACT in terms of team-based care structure, team processes and team effectiveness. Four measures related to team structures: 1) spending at least a half-hour per day in team “huddles” to plan the workday; 2) being assigned to a PACT; 3) being assigned to multiple PACTs; and 4) that the respondent’s PACT was staffed to a recommended ratio of 3.0 FTE team members for each FTE provider.
Measures of team processes included team functioning and delegation of clinical responsibilities. We used a 4-scale measure of team functioning adapted from the Survey of Organizational Attributes of Primary Care.44 It included scales assessing communication about conflict, participatory decision making, stressful work environment, and a history of successful change in the clinic. We developed a 15-item measure to assess the extent to which the PCP delegated and relied on the team to accomplish clinical activities. Items were scored on a 4-point scale from “not at all” to “a great deal.” To create summary scores for delegation, we standardized items using z-scores and performed principal components analysis45 to determine the most efficient representation of the items, resulting in three scores: activities related to direct patient care (e.g., “Educating patients about disease-specific self-care activities”); patient assessments (e.g., “Assessing patient lifestyle factors”); and resolving messages (e.g., “Resolving messages from patients”).
Two items assessed whether the respondent felt they spent the majority of their time working to the top of their competency in terms of 1) doing work that someone with less training could do; and 2) doing work for which they do not have sufficient training. We also included a measure of respondents’ confidence or self-efficacy that their team was capable of implementing the PACT model. A copy of the full survey instrument is included online as Appendix A.
We adjusted for respondents’ length of tenure with VA and supervisory level. We did not include demographics such as gender and race, which have not been consistently associated with burnout.46 We also included three measures of clinic workload and capacity: 1) overall clinic-adjusted average panel size, which is adjusted for type of provider (physician vs. nurse practitioner and physician assistant) and FTE; 2) the proportion of providers in the clinic who are over-capacity, which is whether providers’ panels exceeded the panel size the VA expects a PCP to manage adjusted for provider FTE; and 3) clinical “intensity” of the patients in the panel, which is the average Diagnostic Cost Group (DCG) score. DCG score is based on demographics and weighted diagnoses recorded in a 12-month period. Larger DCG indicates greater complexity.47 We also adjusted for whether the clinic was community-based or co-located with a VA medical center.
Analyses
We conducted a respondent-level, logistic regression of employee burnout (dichotomized as presence of burnout symptoms or not) as a function of PACT implementation related to team-based care, adjusting for respondent characteristics and clinic-level workload characteristics. Analyses were adjusted for clustering by clinic using robust standard errors. The model was specified a priori based on components of team-based care that are goals of the PACT initiative; we did not engage in stepwise regression. For multivariate analyses, we excluded 250 observations that contained “don’t know/not applicable” response options for one or more of the continuous variables comprising the team functioning or delegation of clinical responsibilities scales. For ordinal variables, we included dummy variables for “don’t know/not applicable” responses. We report odds ratios with robust standard errors. All analyses were completed with STATA/MP 11.2 (Stata Corp LP, College Station, TX) and SAS 9.3 (SAS Institute, Inc., Cary, NC).
KEY RESULTS
We received a total of 4,819 surveys (626 clinics) from respondents in the four occupations comprising PACTs (estimated response rate of approximately 25 %). Overall, the prevalence of burnout was 39 %, with the highest prevalence for PCPs (45.4 %), and the lowest for Clinical Associates (31.7 %).
Virtually all independent variables were significantly correlated with burnout, the exceptions being assignment to multiple PACTs, and the clinic workload and capacity variables: proportion of PCPs with panels over-capacity, adjusted panel size and patient intensity. The strongest associations were seen for working to top of competency (< 25 % of time spent on work that someone with less training could do or for which one has too little training), being on a PACT staffed to recommended ratio, collective self-efficacy in ability to implement PACT, and delegation of clinical activities (particularly activities related to direct patient care) (Table 1).
In adjusted multivariate analyses (Table 2), five elements of team-based care remained significantly correlated with burnout: participatory decision making (OR 0.65, 95 % CI 0.57, 0.74), being assigned to a PACT (OR 1.46, 95 % CI 1.11, 1.93), having a team staffed to the recommended 3.0 ratio (OR 0.79, 95 % CI 0.68, 0.93), spending 25–50 % of one’s time on work that could be done by someone with less training (OR 1.29, 95 % CI 1.07, 1.57), and a chaotic work environment where employees feel overwhelmed by work demands (OR 4.33, 95 % CI 3.78, 4.96).
Both longer tenure and occupation were correlated with burnout in adjusted analyses. Those with 2 or more years of tenure had higher odds of burnout relative to those with less than 6 months (OR range 2.13–2.68). Clinical associates (OR 0.74, 95 % CI 0.58, 0.95) had lower odds of burnout relative to PCPs. None of the measures of clinic-level workload, including the proportion of PCPs whose panels were overcapacity, were significantly correlated with burnout.
Findings were similar when we used the ordinal PWS burnout measure and the Maslach Burnout Inventory Emotional Exhaustion scale. When we conducted analyses with independent variables aggregated to the clinic level, being assigned to a fully-staffed teamlet and working to top of competency were no longer significant across all measures of burnout (dichotomized and ordinal PWS, and MBI), but the results were otherwise similar. These results are included in online Appendix B.
CONCLUSIONS
We found that participatory decision making and having recommended staffing levels for primary care teams were associated with significantly lower burnout after adjusting for a variety of characteristics of respondents and clinics. Being assigned to a PACT; a stressful, fast-moving work environment; and spending time on work that someone with less training could do were associated with higher odds of burnout.
This paper makes two important contributions to the limited literature on the association of PCMH implementation with burnout in primary care.24,25,27,28,48 First, this is the first study we know of to assess the association of PCMH implementation with burnout in a broad population of clinics all engaged in implementing a PCMH model, rather than demonstration sites, or sites surveyed on the extent to which they already resemble PCMH models. We also include all members of the team, not just physicians. Consequently, our findings provide a more accurate picture about how a large-scale effort to implement a PCMH model is likely to affect all primary care personnel. Second, while past studies of PCMH initiatives have tested or described changes in burnout, no studies have tested which PCMH elements are associated with burnout among clinics implementing a PCMH model. We are able to identify specific elements of the model that are significant, independent correlates of burnout, which may help other systems embarking on PCMH initiatives.
Respondents who reported being on a team staffed to the recommend 3.0 ratio had significantly lower odds of burnout, even after adjusting for clinic-level workload and the proportion of PCPs whose panels were overcapacity. Our findings suggest that working on a fully staffed team is important for mitigating burnout, and add to a growing body of literature regarding the important impact of medical teams on employee stress, satisfaction and burnout.49 Conversely, having a stressful, fast-moving work environment was associated with more than four times the odds of burnout, even after taking into account being on a team staffed to the recommended ratio and clinic-level measures of workload. Being assigned to a PACT was also associated with higher burnout. This is consistent with previous literature regarding the deleterious effect of a large-scale, organizational change,30,31 but could also be unobserved confounding, as the small proportion of respondents who had not been assigned to a PACT 2 years into the initiative may have been different in other respects as well.
We also found longer tenure was positively associated with burnout. The association with tenure may be a common feature of work life: the longer one spends in a job, the more one is worn out by it. But it may also be a function of the PACT initiative: employees with the longest tenure may experience the stress of major transformation most acutely, because their habits are well established and their expectations most likely to be challenged by the initiative. A question for future research will be to test the interaction of respondent tenure with extent of implementation of the new model, to determine if change-related stress disproportionately affects longer-tenured employees.
LIMITATIONS
The most important limitation is that our findings are based on cross-sectional observations; thus, we cannot draw causal inferences between measures of team-based care related to PACT and employee burnout. It is possible that sites with high rates of burnout are at a disadvantage implementing PACT, or that there is unobserved confounding (e.g., that clinics with adequate staffing and strong cultures of improvement have lower burnout and are better able to implement PACT). As additional data become available, we will examine trends over time to better address the association of changes in PACT implementation with changes in burnout.
There are also two other potential limitations that bear discussion, though we argue that both cases are of limited concern for the purposes of the analyses reported here (i.e., testing the association of specific PACT components with burnout).
First, because both the dependent and independent variables were measured with the same survey instrument, common method bias can inflate associations between variables. However, this is primarily a concern when a single or small number of independent variables are tested, and not for large numbers of independent variables in multivariate regression, where shared variance is not reflected in coefficients or odds ratios.50,51 Furthermore, we obtained nearly identical findings in clinic-level analyses, in which we would expect common method variance to be normally distributed, and as a result, attenuated.
Second, there is a threat of selection bias due to our survey methodology. Because we were obligated to distribute the survey via clinical leadership, and because surveys had to be anonymous, we do not have a defined sampling frame, and it is impossible to know for certain who participated in the survey. The individuals who did participate may differ in important ways from those who did not. However, our sample has very similar demographics with a primary care sample from a general employee survey, the VA All Employee Survey, fielded the month prior to ours, which achieved a 62 % response rate (tables of respective demographics and burnout rates by occupation in online Appendix C); our sample had a higher proportion of supervisors, fewer African Americans, and burnout was 6.6 % higher (38.5 % vs. 31.9 % among the four occupations comprising PACTs). Our sample was also representative of primary care clinics, with 69 % of VA primary care sites nationally being represented in our findings. This gives us added confidence that our findings are generalizable.
In terms of measures, the tenure item included response options that overlap, which may have caused confusion to respondents and introduced measurement error, and the staffing ratio question uses the term “recommended staffing ratio,” which may have introduced social desirability bias.
In summary, our findings suggest that lower burnout may be achieved by a medical home model that includes appropriately staffed teams, emphasizes participatory decision making among team members, and increases the proportion of time team members spend on work well-suited to their training.
REFERENCES
Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–85.
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–93.
Shanafelt T, Sloan J, Satele D, Balch C. Why do surgeons consider leaving practice? J Am Coll Surg. 2011;212:421–2.
Van Bogaert P, Clarke S, Roelant E, Meulemans H, Van de Heyning P. Impacts of unit-level nurse practice environment and burnout on nurse-reported outcomes: a multilevel modelling approach. J Clin Nurs. 2010;19:1664–74.
Linzer M, Manwell LB, Williams ES, et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151(28–36):W6–9.
Landon BE, Reschovsky JD, Pham HH, Blumenthal D. Leaving medicine: the consequences of physician dissatisfaction. Med Care. 2006;44:234–42.
Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27:28–36.
Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–67.
Parker PA, Kulik JA. Burnout, self- and supervisor-rated job performance, and absenteeism among nurses. J Behav Med. 1995;18:581–99.
Sargent MC, Sotile W, Sotile MO, Rubash H, Barrack RL. Quality of life during orthopaedic training and academic practice. Part 1: orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2009;91:2395–405.
Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40:486–90.
Halbesleben JR, Wakefield BJ, Wakefield DS, Cooper LB. Nurse burnout and patient safety outcomes: nurse safety perception versus reporting behavior. West J Nurs Res. 2008;30:560–77.
Spence Laschinger HK, Leiter MP. The impact of nursing work environments on patient safety outcomes: the mediating role of burnout/engagement. J Nurs Adm. 2006;36:259–67.
West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302:1294–300.
Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000.
Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122–8.
Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manag Rev. 2008;33:29–39.
Argentero P, Dell’Olivo B, Ferretti MS. Staff burnout and patient satisfaction with the quality of dialysis care. Am J Kidney Dis. 2008;51:80–92.
Aiken LH, Clarke SP, Sloane DM, et al. Nurses’ reports on hospital care in five countries. Health Aff. 2001;20:43–53.
Freeborn DK. Satisfaction, commitment, and psychological well-being among HMO physicians. West J Med. 2001;174:13–8.
Graber JE, Huang ES, Drum ML, et al. Predicting changes in staff morale and burnout at community health centers participating in the health disparities collaboratives. Health Serv Res. 2008;43:1403–23.
Alexander JA, Bae D. Does the patient-centered medical home work? A critical synthesis of research on patient-centred medical homes and patient-related outcomes. Health Serv Manag Res. 2012;25:51–9.
Jackson GL, Powers BJ, Chatterjee R, et al. The patient-centered medical home: a systematic review. Ann Intern Med. 2013;158:169–78.
Reid RJ, Coleman K, Johnson EA, et al. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood). 2010;29:835–43.
Reid RJ, Fishman PA, Yu O, et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manage Care. 2009;15:e71–87.
Hochman ME, Asch S, Jibilian A, et al. Patient-centered medical home intervention at an internal medicine resident safety-net clinic. JAMA Intern Med. 2013. doi: 10.1001/jamainternmed.2013.9241. [Epub ahead of print].
Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaen CR. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the National Demonstration Project. Ann Fam Med. 2010;8(1):S45–56. S92.
Lewis SE, Nocon RS, Tang H, et al. Patient-centered medical home characteristics and staff morale in safety net clinics. Arch Intern Med. 2012;172:23–31.
Abrahamson E. Change Without Pain: How Managers Can Overcome Initiative Overload, Organizational Chaos, and Employee Burnout. Watertown, MA: Harvard Business Press; 2004.
Bambra C, Egan M, Thomas S, Petticrew M, Whitehead M. The psychosocial and health effects of workplace reorganisation. 2. A systematic review of task restructuring interventions. J Epidemiol Community Health. 2007;61:1028–37.
Klein S. The Veterans Health Administration: implementing patient-centered medical homes in the nation’s largest integrated delivery system. Commonw Fund Publ. 2011;1537:16.
Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manage Care. 2013;19:e263–72.
Helfrich CD, Dolan E, Fihn SD, Rodriguez HP, Meredith LS, Rosland AM, Lempa M, Wakefield BJ, Joos S, Stark R, Schectman G, Nelson K. Patient centered medical home implementation and burnout at VA clinics. J Gen Inter Med. Under revision.
PACT Demonstration Laboratory Coordinating Center. Return on Investment in VA PACT Implementation: Preliminary Report to the Office of the Secretary of Veterans Affairs. Seattle: Veterans Health Administration; 2013.
Mohr D, Schectman G, Helfrich CD. Trends in job satisfaction and workplace climate in VA primary care relative to in-patient care. J Gen Inter Med. Under review.
Dyrbye LN, West CP, Satele D, Sloan JA, Shanafelt TD. Work/home conflict and burnout among academic internal medicine physicians. Arch Intern Med. 2011;171:1207.
Linzer M, Visser MR, Oort FJ, Smets E, McMurray JE, de Haes HC. Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med. 2001;111:170–5.
Aiken LH, Sloane DM. Effects of organizational innovations in AIDS care on burnout among urban hospital nurses. Work Occup. 1997;24:453–77.
Schmoldt RA, Freeborn DK, Klevit HD. Physician burnout: recommendations for HMO managers. HMO Pract. 1994;8:58–63.
Williams ES, Konrad TR, Linzer M, et al. Physician, practice, and patient characteristics related to primary care physician physical and mental health: results from the Physician Worklife Study. Health Serv Res. 2002;37:121–43.
Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20:75–9.
Leiter MP, Shaughnessy K. The Areas of Worklife Model of burnout: tests of mediation relationships. Ergonomia Int J. 2006;28:327–41.
Dolan E, Helfrich C, Nelson K, et al. Substantiation of a single-item burnout measure in a sample of VHA primary care clinical staff. In: AcademyHealth Annual Research Meeting. Baltimore, MD; 2013.
Ohman-Strickland PA, John Orzano A, Nutting PA, et al. Measuring organizational attributes of primary care practices: development of a new instrument. Health Serv Res. 2007;42:1257–73.
Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. New York, NY: McGraw-Hill Inc.; 1994.
Maslach C, Leiter MP. Early predictors of job burnout and engagement. J Appl Psychol. 2008;93:498–512.
Stefos T, Burgess JF, Mayo-Smith MF, et al. The effect of physician panel size on health care outcomes. Health Serv Manag Res. 2011;24:96–105.
Nutting PA, Crabtree BF, Miller WL, Stange KC, Stewart E, Jaen C. Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff. 2011;30:439–45.
Buttigieg SC, West MA, Dawson JF. Well-structured teams and the buffering of hospital employees from stress. Health Serv Manag Res. 2011;24:203–12.
Doty DH, Glick WH. Common methods bias: does common methods variance really bias results? Organ Res Methods. 1998;1:374–406.
Siemsen E, Roth A, Oliveira P. Common method bias in regression models with linear, quadratic, and interaction effects. Organ Res Methods. 2010;13:456–76.
Acknowledgements
Our thanks to Julie Kurutz and John Witzlib of the VA Healthcare Analysis and Information Group (HAIG) for fielding the survey; to John Messina for assistance with communication, scheduling, and data tables; and to members of the PACT Demonstration Laboratory Coordinating Center Organizational Function Working Group who contributed invaluable expertise and feedback.
This work was undertaken as part of the VA’s PACT Demonstration Laboratory initiative, supporting and evaluating VA’s transition to a patient-centered medical home. Funding for the PACT Demonstration Laboratory initiative is provided by the VA Office of Patient Care Services. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 326 kb)
Rights and permissions
About this article
Cite this article
Helfrich, C.D., Dolan, E.D., Simonetti, J. et al. Elements of Team-Based Care in a Patient-Centered Medical Home Are Associated with Lower Burnout Among VA Primary Care Employees. J GEN INTERN MED 29 (Suppl 2), 659–666 (2014). https://doi.org/10.1007/s11606-013-2702-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2702-z